Center introduction
~Sapporo High Functioning Radiotherapy Center SAFRA~
Sapporo Kojinkai Memorial Hospital, which has the latest diagnostic devices and treatment equipment, is located in Sapporo, Hokkaido. This advanced acute-care hospital has 276 beds and treats mainly cancer, cerebrovascular diseases, heart diseases and motor system diseases. Using the latest equipment and treatments, we provide cutting-edge medical care.
Our hospital promotes multidisciplinary cancer treatment that effectively combines multiple therapeutic procedures (surgery, chemotherapy, immunotherapy, radiotherapy). Multidisciplinary cancer treatment requires cooperation among multiple clinical departments and centers. Among them, the Sapporo High Functioning Radiotherapy Center (SAFRA) plays a central role in“ body-friendly non-surgical treatment,” which is our hospital’s mission. We hope to enable patients to live their day-to-day lives while undergoing cancer treatment.
Radiotherapy equipments at SAFRA
CyberKnife is a radiotherapy system that consists of a high-precision robot arm of the kind used in precision industries and a small linear accelerator (Linac).

Using a freely moving robot arm, CyberKnife irradiates the target lesion from different directions. Its pinpoint irradiation of the target lesion minimizes radiation exposure to the surrounding normal tissue, affording fewer side effects and allowing elderly people and those who are frail to receive treatment. The system enables the pinpoint irradiation to be applied for risky cases in which surgery is difficult, and it enables lesions with an irradiation history to be re-irradiated. The choice between stereotactic radiotherapy and intensity-modulated radiotherapy depends on the treatment region and lesion.
For positioning, CyberKnife uses X-ray images taken by two X-ray photography devices installed on the ceiling. Position gaps are corrected by using a bed with six joints, called RoboCouch, and a robot arm. Even during irradiation, X-ray images are taken at regular intervals for localization. During treatment, position gaps are calculated for correction, and adjustments are made by the robot arm. These procedures enable accurate positioning and position correction, as well as advanced pinpoint irradiation.
This method is used for the head region, a region for which CyberKnife excels. The system recognizes the boundaries between the skull bones and the air and positions the entire head. Each patient wears a custom-made mask called a“ shell.”
When the trunk is treated, the vertebral body (backbone) is used for positioning. This method is especially effective when the lesion to be irradiated is in or near the vertebral body.
A metal marker embedded in the body is used for positioning. This method is used for regions away from the vertebral body as well as for the lungs and liver, where positioning based on X-ray images is difficult. A metal marker is placed in the body before treatment.
At our hospital, CyberKnife can track and irradiate a lesion in the lung, liver o r pancreas that moves with respiration.* This can reduce the radiation exposure of normal tissue. Patients are not required to hold their breath. They can receive treatment while breathing normally.
*For some lesions. a metal marker is placed before treatment is administered.
In cases where X-ray images can be used to visualize a lesion in the lung for positioning, a moving body can be tracked without using a metal marker. In addition to positioning using the vertebral body, the lesion is used as a marker to maintain positional accuracy. High-precision treatment can be provided without a metal marker if a pre-treatment simulation shows favorable results.*
*However, this method is limited to the irradiation of lesions in the lung.
CyberKnife can deliver a high dose of radiation in each treatment. The duration of each treatment session is 30 to 60 minutes, including positioning, and the treatment is completed in one to several sessions. Outpatient treatment is usually possible. However, hospitalization may be recommended for certain medical conditions.
After the treatment, periodic imaging tests are conducted for follow-up. Follow-up observation may be made at another facility.
TomoTherapy is a versatile radiotherapy system that uses a small linear accelerator (Linac) embedded in a CT scanner.

TomoTherapy is characterized by intensity-modulated radiotherapy, which is an effective treatment that has fewer side effects. In this irradiation method, the beam shape and irradiation time are varied according to the position and angle of irradiation. Various radiation beams overlap, causing the intensity of radiation to differ at those overlapping points. This makes it possible to deliver a high dose of radiation to the target site while limiting the radiation exposure of surrounding normal tissue. The number of fine beams per treatment site can exceed 10,000. Considering that there are also IMRT machines with beam numbers of 100 or so, TomoTherapy can be described as a high-end IMRT model. Radiotherapy plans involving TomoTherapy that save normal tissue and deliver high doses of radiation to the target provide accurate, beautiful distribution charts of radiation that cannot be achieved with other treatment systems.
Another characteristic of TomoTherapy is CT image-guided radiotherapy (CT-IGRT), which enables accurate positioning. Even when high-precision irradiation is possible, position gaps affect the therapeutic efficacy and side effects. TomoTherapy efficiently combines a CT scanner and a radiotherapy unit to provide high-precision positioning. A CT image is taken just before each irradiation to accurately determine the position of the target. If the gap is large, the position is corrected automatically or manually for high-precision irradiation. Unlike X-ray images, in which bones and markers are used for positioning, the target in the body and the situation of the surrounding tissue (e.g., the movements of breathing and of the intestinal tract, the size of the bladder and the stomach) are clarified by CT for positioning. This is the most direct and accurate IGRT system.
Moreover, TomoTherapy enables spiral irradiation, which is not possible with other IMRT systems. Spiral irradiation is achieved by slowly moving the bed of the patient through beams that rotate at an extremely high speed while changing their shape (photo). When high-precision IMRT is used in a spiral manner, successive multiple targets can be irradiated consecutively and targets in a wide area can be irradiated uniformly. Like radiotherapy after breast-conserving surgery, fixed-angled irradiation is also possible (fixed direct irradiation). With TomoTherapy, even fixed-angle irradiation can limit the side effects on the lung and the heart because fine beams overlap.
The time required for a TomoTherapy session varies depending on the treatment range and site, but it is estimated to be approximately 20 minutes, including CT scanning and confirmation. The number of sessions also depends on the site, but it is comparable to that for conventional radiotherapy. Outpatient treatment is usually possible. However, hospitalization may be recommended for certain medical conditions. After the treatment, periodic imaging tests are conducted as follow-up. The follow-up observation may be made at another facility.
Proton therapy is attracting world attention as a cutting-edge particle beam treatment. ProteusOne, which our hospital has introduced, is the latest model from IBA, the leading manufacturer of proton therapy systems. Our hospital is the 15th facility in Japan to offer proton therapy and the only facility in Japan with CyberKnife, TomoTherapy and a proton therapy system*. * as of Junuary 2020

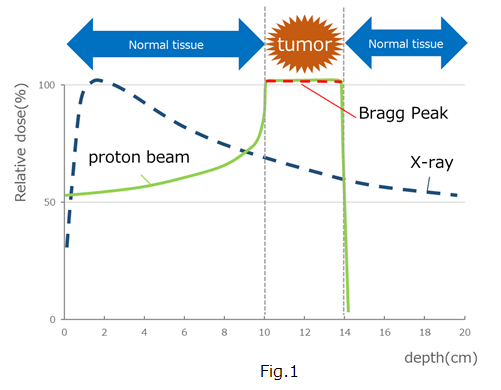
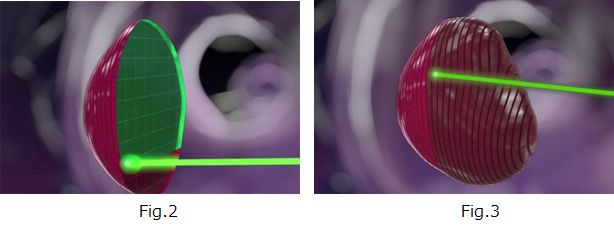
Our hospital has introduced the IBA Proton Beam Therapy System "Proteus One".With this device, a proton beam is irradiated to scan (scanning) the tumor with a thin beam called a "pencil beam" of about 3-4 mm as shown in Fig.2 below.Intensity-modulated proton beam therapy (IPMT) using scanning with a pencil beam irradiates even normal tumors with three-dimensionally stacked proton beams, as shown in Fig. 3, to the surrounding normal tissue. Tumors can be given an effective dose while minimizing the effects of.
If you have any questions, please feel free to ask.
Major diseases amenable to these treatments
|
Head and neck
|
Spine and spinal cord
|
Breast and abdomen
|
Pelvis
|
*In addition to those mentioned above, there are other diseases that are amenable to treatment.
It is necessary to check and study the clinical history and the results of various tests. Please contact us.
Access & Inquiry
Miyanosawa 2-jo 1-chome 16-1, Nishi-ku, Sapporo, 063-0052
Phone number for SAFRA: 011-676-7419
E-mail: safra@kojinkai.or.jp
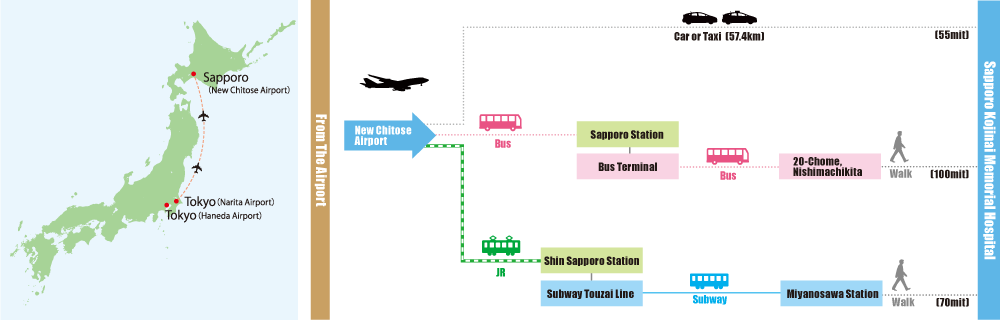
 By air |
From Narita Airport or Haneda Airport to New Chitose Airport |
|---|
 By bus |
From New Chitose Airport International Terminal to Sapporo Station, then from Sapporo Station Bus Terminal to Nishimachi Kita 20-chome (approx. 100 min.) |
|---|---|
 By JR train |
From New Chitose Airport to Shin-Sapporo, then change to the Tozai Subway Line and get off at Miyanosawa (approx. 70 min.) |